Diabetes is a chronic condition that affects millions of people worldwide. While the condition can be managed with proper care and medication, one of its significant complications is the increased risk of chronic wounds. These persistent, non-healing wounds can be painful, prone to infection, and difficult to manage. In this article, we’ll explore the connection between diabetes and chronic wounds, why individuals with diabetes are more susceptible, and how to manage and prevent them.
What Are Chronic Wounds?
A chronic wound is any injury or sore that does not heal within a reasonable timeframe—typically more than 3 months. Chronic wounds may remain in a prolonged inflammatory stage or become stalled in the healing process, making it difficult for the body to repair damaged tissue. Common types of chronic wounds include:
- Diabetic foot ulcers
- Pressure ulcers (bedsores)
- Venous leg ulcers
- Arterial ulcers
For individuals with diabetes, the chronic wound cycle can be particularly challenging. Healing is often slow, and even small cuts or blisters can develop into serious, non-healing ulcers.
Why Do People with Diabetes Develop Chronic Wounds?
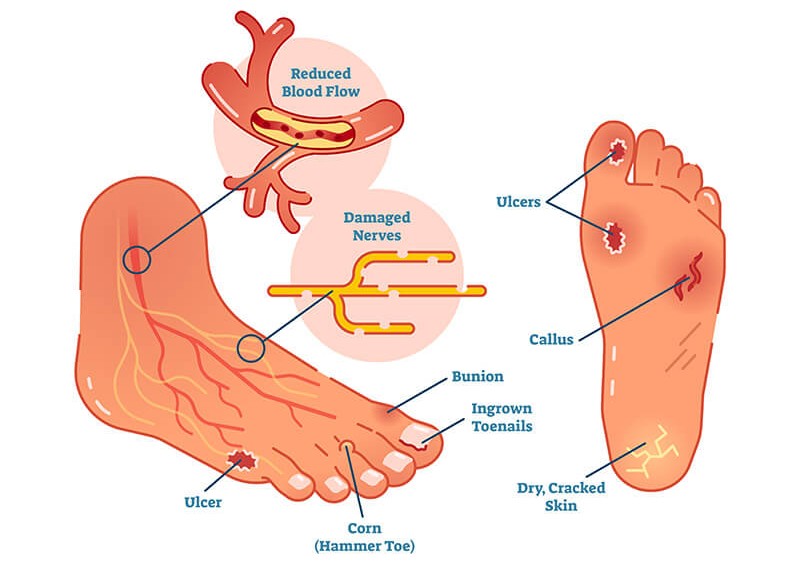
Diabetes affects wound healing in several ways. If blood sugar levels are poorly controlled, it can create a domino effect that impairs multiple bodily functions necessary for efficient healing. Here are the primary reasons why chronic wounds are more common in people with diabetes:
1. Impaired Circulation
One of the most significant factors contributing to chronic wounds in diabetics is poor circulation. Over time, high blood sugar levels can damage blood vessels, leading to peripheral vascular disease (PVD), which restricts blood flow to the extremities. This impaired circulation slows down the delivery of oxygen and nutrients essential for wound healing, making it harder for the body to repair damaged skin and tissue.
What you can do:
- Manage blood sugar levels through diet, exercise, and medication.
- Engage in physical activity to promote better circulation.
- Avoid smoking, which can further constrict blood vessels.
2. Diabetic Neuropathy (Nerve Damage)
Diabetes can also cause neuropathy (nerve damage), particularly in the feet and legs. Neuropathy reduces sensation, meaning that individuals may not feel the pain or discomfort from a cut, blister, or pressure point. Because of this, wounds in these areas can go unnoticed and untreated, allowing them to develop into more serious issues, such as diabetic foot ulcers.
What you can do:
- Inspect your feet regularly, especially the soles and areas between the toes, to catch any wounds early.
- Use cushioned, well-fitted shoes to reduce the risk of friction and pressure sores.
- If you have diabetic neuropathy, work with a healthcare provider to develop a comprehensive foot care plan.
3. Weakened Immune System
High blood sugar levels can suppress the immune system, making it harder for the body to fight infections. This is particularly concerning when dealing with chronic wounds, as infections can quickly complicate the healing process and even lead to severe consequences like gangrene or amputation.
What you can do:
- Keep blood sugar levels within the recommended range.
- Maintain a clean and sterile environment around wounds.
- Seek medical attention at the first sign of infection (redness, swelling, pus, or warmth around the wound).
4. Slower Tissue Regeneration
For diabetics, the healing process itself is often impaired. Chronic high blood sugar levels can slow down the production of collagen, a key protein involved in tissue repair. This means that wounds take longer to heal, and the healing tissue may be weaker and more susceptible to re-injury.
What you can do:
- Eat a diet rich in protein, vitamin C, and zinc, which support collagen production and tissue regeneration.
- Stay hydrated to support overall bodily functions and wound healing.
Common Chronic Wounds in Diabetic Patients
Chronic wounds in individuals with diabetes typically manifest in specific areas of the body, particularly the feet. Below are the most common types:
1. Diabetic Foot Ulcers
Diabetic foot ulcers are one of the most common and severe types of chronic wounds associated with diabetes. They often develop due to neuropathy, which causes loss of sensation in the feet. These ulcers may begin as small blisters or cuts but can grow larger and deeper if left untreated. Poor circulation also impairs healing, which makes diabetic foot ulcers highly prone to infection.
What you can do:
- Inspect feet daily for cuts, blisters, or signs of infection.
- Ensure proper foot hygiene and keep feet dry.
- Wear shoes that fit well and provide adequate support.
2. Pressure Ulcers (Bedsores)
People with diabetes who spend extended periods in bed or a wheelchair are at risk of developing pressure ulcers, also known as bedsores. These ulcers form when prolonged pressure on specific areas of the body (like heels, buttocks, or elbows) restricts blood flow to the skin. In diabetics, these ulcers are more likely to become chronic due to circulation issues and poor healing capacity.
What you can do:
- Reposition regularly to relieve pressure points.
- Use pressure-relieving devices like cushions or specialized mattresses.
- Keep skin clean and dry to avoid moisture-related skin damage.
3. Venous Leg Ulcers
These ulcers develop due to venous insufficiency, where blood flow from the legs back to the heart is impaired, leading to pooling of blood in the lower extremities. For diabetics with poor circulation, venous leg ulcers can be a significant risk.
What you can do:
- Elevate legs when resting to improve circulation.
- Wear compression stockings as advised by a healthcare provider.
- Keep skin moisturized to prevent dryness and cracking.
Managing Chronic Wounds in Diabetic Patients
While chronic wounds in diabetics can be more challenging to manage, it is possible to heal and prevent complications with proper care. Here are some steps to improve wound healing and minimize risk:
1. Blood Sugar Control
Controlling blood sugar levels is the most important step in preventing and healing chronic wounds. Uncontrolled blood sugar can cause a delay in healing and increase the risk of infection. Aim to keep your blood glucose levels within a healthy range through diet, exercise, and medications as prescribed by your doctor.
2. Wound Care and Cleaning
Keep wounds clean to prevent infection. Follow a healthcare provider’s instructions on dressing changes and use recommended wound care products, such as antimicrobial dressings. It’s crucial to protect the wound from contaminants and avoid putting pressure on it.
3. Regular Foot Inspections
If you have diabetes, check your feet every day for cuts, blisters, redness, or swelling. Because you may not feel injuries due to neuropathy, it’s important to inspect your feet carefully or have someone else help.
4. Seek Professional Care
For chronic wounds that don’t improve, seek treatment from a wound care specialist. Advanced therapies, such as negative pressure wound therapy (NPWT) or skin substitutes, may be needed to accelerate healing.